January premiums reflect new rates, up 6% to nearly $27,000 for family coverage. Here's what's driving increases and how to manage the cost.
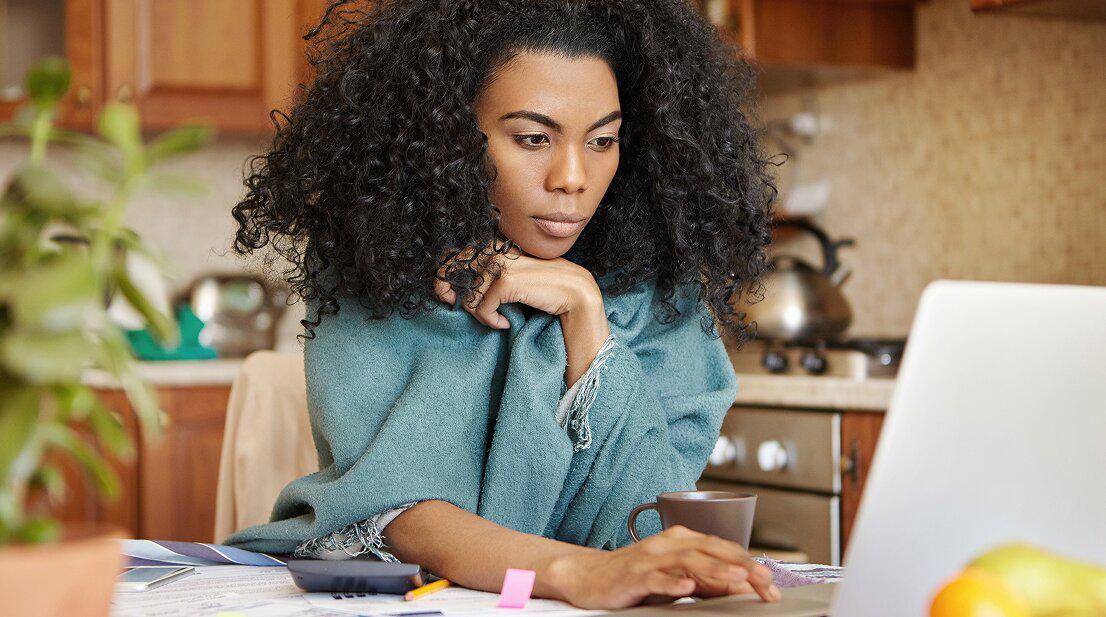
Your first insurance bill of the year just hit, and you’re staring at a number that’s hundreds higher than December’s. What the hell happened?
You’re not imagining it. Family premiums jumped 6% this year, your deductible reset to zero, and your new FSA contributions just kicked in. January is a perfect storm.
Why it hurts: Employer-sponsored family premiums hit $26,993 in 2025[1]. Your share: $6,850/year — about $571/month coming out of your paycheck. That’s before you’ve paid for a single doctor’s visit.
↑ TopWhy January Hits Different
It’s not just higher premiums. January piles on three cost increases at once:
- Your premium went up. Rates increased 6% this year, and that’s hitting your first paycheck now.
- Your deductible reset. That $1,886 average you spent meeting last year’s deductible? Back to zero. You’re paying full price for medical care until you hit it again.
- Your FSA deductions started. If you elected to contribute, those dollars come out before you see them.
This is why January’s paycheck feels so much smaller — and why medical bills sting more until you’ve rebuilt your deductible cushion.
Table of Contents
- The 2025 Premium Picture
- What’s Driving These Increases
- What You Can Do About This Bill
- When Premiums Become Unaffordable
- When You Can’t Absorb the Hit
↑ TopThe 2025 Premium Picture
Most people underestimate how much their employer plan actually costs — because they only see their share. Here’s what you’re actually paying[1]:
| Coverage Type | Annual Premium | Worker Share | Monthly Worker Cost |
|---|---|---|---|
| Family coverage | $26,993 | $6,850 | ~$571 |
| Single coverage | $8,951 | ~$1,400 | ~$117 |
These figures represent employer-sponsored insurance, which covers roughly 155 million Americans. If you’re paying for individual or Marketplace coverage, your costs may differ. For Marketplace plans, CMS reports average premiums for 2026 will be approximately $50 per month after tax credits, up $13 from the previous year[2]. Tax credits cover 91% of the lowest-cost plan premium on average, and enhanced credits under the Inflation Reduction Act continue through 2025.
↑ TopWhat’s Driving These Increases
Your premium didn’t go up randomly. Here’s what’s pushing costs higher:
- Healthcare costs keep climbing. Hospital stays, physician services, and prescription drugs all cost more than last year.
- GLP-1 drugs. The explosion in weight loss and diabetes medications like Ozempic and Wegovy is a major factor in 2025 premium calculations[1].
- Post-pandemic catch-up. People deferred care during COVID. Now they’re getting procedures done, and insurers are paying out more.
These are structural issues — they’re not going away next year. The question is what you can do about THIS bill.
↑ TopWhat You Can Do About This Bill
Review your plan options. If open enrollment hasn’t closed, compare total costs (premiums + deductible + expected out-of-pocket). HDHPs mean lower premiums but higher costs when you need care—best for healthy people. Traditional PPO/HMO plans cost more monthly but offer predictability.
Maximize your HSA. If you have an HDHP, every dollar you contribute reduces your taxable income. 2025 limits: $4,300 (self-only) or $8,550 (family)[3]. Unlike FSAs, these funds never expire.
Claim all eligible tax credits. If you have Marketplace coverage, make sure you’re receiving all credits you qualify for. Update your application if your circumstances have changed.
Budget for Q1. January through March sees higher out-of-pocket spending as you meet new deductibles. Set aside funds for medical expenses and time elective care strategically.
Use preventive care first. Most plans cover preventive care at 100% with no deductible—annual physicals, screenings, vaccinations, well-child visits. You get full value regardless of deductible status.
Check your pay stub. If January’s paycheck is smaller than expected, compare it to last year’s. If deductions don’t match what you elected, contact HR—errors happen.
↑ TopWhen Premiums Become Unaffordable
If health insurance premiums are genuinely unaffordable, you have options:
- Check Marketplace eligibility. Even with employer coverage, you may qualify for subsidized Marketplace plans if your employer plan costs too much relative to your income.
- Review Medicaid eligibility. Life changes (job loss, income reduction) can make you newly eligible. Most states have expanded coverage.
- Ask about payment plans. Some insurers and employers offer premium payment plans. For medical bills, you can often negotiate arrangements directly with providers.
↑ TopWhen You Can’t Absorb the Hit
Between higher premiums, reset deductibles, and post-holiday expenses, January can stretch any budget.
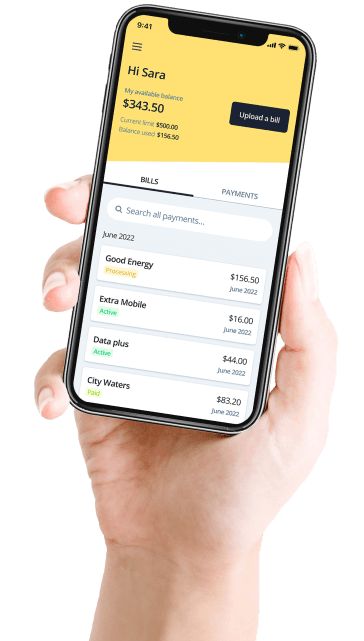
If medical bills are piling up while you’re meeting your new deductible, you can split them into 4 payments over 8 weeks with Deferit. We pay your provider on time while you pay us back. See if you qualify.
↑ TopReferences
- KFF. “2025 Employer Health Benefits Survey.” Kaiser Family Foundation. October 2025.
- Centers for Medicare & Medicaid Services. “Health Insurance Marketplace 2026 Open Enrollment Data."
- Internal Revenue Service. “Publication 969: Health Savings Accounts and Other Tax-Favored Health Plans.” IRS.gov. 2025.